How has COVID-19 affected allergy/immunology clinical services like spirometry, peanut OIT and testing for COVID-19? What are the challenges related to practice staffing? And perhaps most importantly, what have allergists told us about their experiences during COVID-19 and the suggestions they have for other allergy practices? This article will provide some answers as we review this data from the College’s August survey on the impact of COVID-19 on allergy/immunology practices. This is a follow-up to last week’s Insider survey results article that focused on the impact on patient volumes, safety and practice finances.
As a reminder, a total of 3,416 members received the survey and 8.5% completed it. The survey was open from July 30 – August 16. 94% of survey participants were providers, and 80% were in practices with five or fewer allergy/immunology providers. 70% were in private practice-single specialty, 11% were from private practice-multispecialty groups, 8% were academic and 7% were from integrated health systems.

Spirometry
One of the biggest questions allergists have had during COVID-19 is how and whether to do spirometry. More than half of August survey respondents indicated they are conducting spirometry in their offices.
| Are you conducting spirometry in your office? (244 responses) |
# of Responses | % |
|---|---|---|
| Yes | 131 | 54% |
| No | 113 | 46% |
| Source: ACAAI COVID Member Survey 7/30/20 – 8/16/20. Copyright 2020. Data is protected by ACAAI copyright and is prohibited to be shared or published without ACAAI’s consent. | ||
For more survey details on the use of spirometry, including what precautions allergists are taking specific to spirometry, view our recent article Spirometry During COVID-19.
Peanut Oral Immunotherapy (OIT)
- 11% of survey respondents indicated they are currently offering FDA-approved peanut OIT.
- More than 16% are currently offering non-FDA-approved peanut OIT; 9.4% said they plan to eventually offer FDA-approved peanut OIT.
- Close to 73% of respondents said they are not currently offering any form of peanut OIT; 31% do have plans to offer it eventually.
| Which statement most accurately reflects your practice’s plan regarding FDA-pproved oral immunotherapy to peanut? (256 responses) |
# of Responses | % |
|---|---|---|
| Currently offering FDA-approved OIT | 28 | 10.9% |
| Currently offering non-FDA-approved OIT; NO plans to offer FDA-approved OIT | 18 | 7.0% |
| Currently offering non-FDA-approved OIT; DO HAVE plans to offer FDA-approved OIT | 24 | 9.4% |
| Not currently offering OIT and no plans to offer | 106 | 41.4% |
| Not currently offering OIT but DO HAVE plans to offer | 80 | 31.3% |
| Source: ACAAI COVID Member Survey 7/30/20 – 8/16/20. Copyright 2020. Data is protected by ACAAI copyright and is prohibited to be shared or published without ACAAI’s consent. | ||
For those planning on offering FDA-approved peanut OIT, we asked if the COVID-19 pandemic has affected their implementation timeline.
- 31% of respondents said they don’t intend to offer it. (Note the total number of responses to this question, 218, is much lower than that for the previous question, 256. Members with no intention of doing peanut OIT may have skipped this question, thereby undercounting the number that don’t plan to offer it.)
- Only 6% of respondents said it had no impact on their implementation schedule.
- A whopping 39% said it delayed implementation indefinitely, while 24% said it delayed it by 0-6 months.
| If you plan on offering FDA-approved OIT, how has the pandemic affected your implementation timeline? (218 responses) |
# of Responses | % |
|---|---|---|
| No effect on our implementation | 13 | 6.0% |
| Delayed by 0-3 months | 20 | 9.2% |
| Delayed by 3-6 months | 32 | 14.7% |
| Indefinite delay in implementation | 85 | 39.0% |
| I don’t plan on offering FDA-approved OIT | 68 | 31.2% |
| Source: ACAAI COVID Member Survey 7/30/20 – 8/16/20. Copyright 2020. Data is protected by ACAAI copyright and is prohibited to be shared or published without ACAAI’s consent. | ||
COVID-19 Testing
When asked if they were providing any type of COVID-19 testing in their office, 101 out of 291 respondents, or 35%, said they were. Of those, 80% were doing send-out antibody testing, 13% were doing in-house antibody testing, and 39% were doing COVID diagnostic testing.
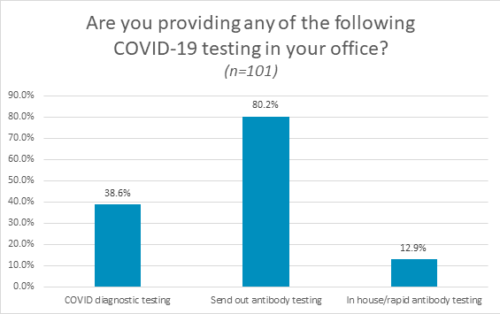
Source: ACAAI COVID Member Survey 7/30/20 – 8/16/20. Copyright 2020. Data is protected by ACAAI copyright and is prohibited to be shared or published without ACAAI’s consent.
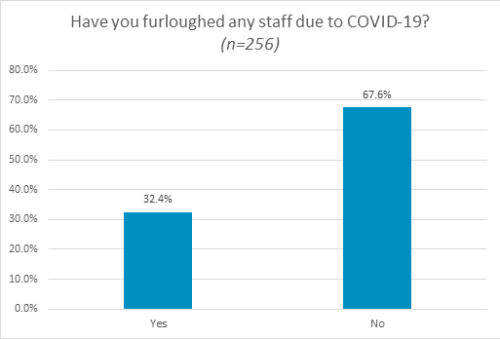
Staffing Issues
When asked if they have furloughed any staff due to COVID-19, a third of respondents said yes.
Source: ACAAI COVID Member Survey 7/30/20 – 8/16/20. Copyright 2020. Data is protected by ACAAI copyright and is prohibited to be shared or published without ACAAI’s consent.
- 209 respondents, or 72% of those taking the survey, reported at least one staff-related issue due to COVID-19.
- The most common issue, reported by 57% of those answering this question, was employee childcare issues impacting work schedules.
- 44% reported staff being exposed to COVID-19 and having to get tested and/or quarantine.
- 30% said an employee preferred not to work because they or someone in their family was in a high-risk category.
| Which of the following staff-related issues are you experiencing or have you experienced? (Check all that apply) (240 responses) |
# of Responses | % |
|---|---|---|
| Employee childcare issues impacting work schedules | 136 | 56.7% |
| Staff exposed to COVID-19 and need to quarantine/get tested | 105 | 43.8% |
| Employee and/or their family are in high-risk category and prefer not to work | 73 | 30.4% |
| Employees electing to stay on unemployment rather than return to office | 53 | 22.1% |
| Difficulty attracting employees to work in medical office | 48 | 20.0% |
| Not sure | 31 | 12.9% |
| Other | 26 | 10.8% |
| Source: ACAAI COVID Member Survey 7/30/20 – 8/16/20. Copyright 2020. Data is protected by ACAAI copyright and is prohibited to be shared or published without ACAAI’s consent. | ||
Practice Pearls
Survey respondents were asked if they had advice to share on how best to continue providing quality allergy and asthma care during COVID-19. 62 people provided suggestions.
The most common response (26%) involved implementing and following safety protocols (PPE, hand washing, social distancing, pre-screening patients). Two people mentioned testing for COVID-19 prior to doing procedures like FeNO and PFT.
7 people said telemedicine was important to their practice.
- “Be very patient with telemedicine. We always reassure patients we can see them in the office if they desire or if we think it is clinically needed.”
- “Telehealth appointments work and are decreasing patient anxiety about leaving home.”
Several people mentioned remaining flexible, patient and willing to learn from others.
- “Be patient. Realize the day is not going to go as smoothly as usual. Reinvent some of the things you do. Remember, allergists have the most ingenuity of any group of physicians!”
- “Be willing to go outside your comfort level to maintain some form of workflow.”
Some had innovative ideas:
- Install a doorbell or create a system where patients call when at the office. You can alert them by phone when you are ready for them to come in.
- Have patients use the ACT score to help asthma control and report to allergist via email.
- Revise your schedule to align with the number of rooms available and the type of visit to keep waiting times short.
- Install negative airflow exhaust fans in exam, testing and PFT rooms providing complete air exchange every 5-7 minutes.
Several respondents noted the importance of clear patient communication/education about COVID-19 and practice safety protocols.
Several respondents emphasized frequent communication with staff, plus repeated training on policies and procedures put in place for COVID-19.
- “Daily conferences with the entire staff before seeing patients has kept us communicating, reducing stress and supporting each other.”
This is clearly still a challenging time for many allergy/immunology practices. Even in this difficult time, however, some allergists remain hopeful. “I hear over and over how thankful patients are that I am open and available to them. We need to remember why we first decided we wanted to be physicians. For many of us, that was in a time when we knew far less about infectious disease than we do today.”
Know that you are not alone; many practices are facing the same challenges. The College is here to support you and provide guidance and resources for the necessary practice changes in response to this pandemic. We will work with members to identify ways to “crisis-proof” your allergy practice in the future.
Please access our COVID-19 resource page for clinical, coding, telemedicine, practice management and patient resources to assist you. We encourage you to reach out to your colleagues through DocMatter to share your experiences. The College would like to thank Drs. Andrew Nickels, Grace Tamesis and Payel Gupta for their work on this survey. We extend special thanks to Dr. Tamesis for her assistance on this article.


